


Mine Health and Safety Act, 1996 (Act No. 29 of 1996)NoticesGuideline for the Compilation of a Mandatory Code of Practice for the Prevention, Mitigation and Management of COVID-19 outbreakAnnexuresAnnexure 6: Guidance on PPE for the COVID-19 pandemic |
| ANNEXURE 6: | Guidance on PPE for the COVID-19 pandemic |
(For information purposes)
GUIDANCE ON PERSONAL PROTECTIVE EQUIPMENT FOR COVID-19 PANDEMIC
21 April 2020
| 1. | INTRODUCTION |
The global COVID-19 pandemic was recorded for the first time in South Africa on 5th March. Since then the country and industry have had to adjust the world of work drastically, resulting in a state of disaster and lockdown in the country from 26th March to 30th April 2020. This guidance is specifically directed at the use of additional personal protective equipment (PPE) for COVID-19.
| 2. | PURPOSE AND SCOPE |
This document provides recommendations for the proper use of personal protective equipment (PPE) for specific situations, to protect employees in the South African Mining Industry (SAMI) against exposure to the coronavirus (SARS-CoV-2) called COVID-19 and airborne pollutants in the workplace. In every situation, employees may be placed in a unique exposure risk, so the recommendations are designed to ensure that the most appropriate and effective PPE to suit a specific situation. The document does not change any current practices regarding PPE that has been previously issued to employees based on the risk assessed by the employer. It Is still the duty of the employer to assess any risk and the guidance is meant to assist the employer in deciding on the best PPE to be adopted for protection of employees against COVID-19.
| 3. | RATIONALE FOR GUIDANCE DOCUMENT: CORONAVIRUS TRANSMISSION |
The SARS-CoV-2 virus (COVID-19) is spread through respiratory droplets and contact with contaminated surfaces. The virus can be transmitted from infected people by cough and sneeze droplets, which land on surfaces and hands. A person can become infected if they inhale coughed or sneezed infectious droplets, or by touching contaminated surfaces and then touching their eyes, nose, or mouth without washing their hands. COVID-19, airborne transmission may be possible in specific circumstances and settings in which procedures or support treatments that generate aerosols are performed, e.g., spirometry, alcohol testing, invasive medical procedures, cardiopulmonary resuscitation and removal of cardio-thoracic organs for compensation purposes.
| 4 | MINIMUM PRECAUTIONARY MEASURES AGAINST INFECTION |
| (a) | Social distancing must be at least 1 (one) metre away where possible. |
| (b) | Wash hands with soap and water for 20 seconds, or use alcohol-based hand sanitiser after contact with any person or after contact with frequently touched surfaces e. g. phones, door handles etc. |
| (c) | Wiping workstation equipment with a disinfect (such as a 0.1% bleach solution) pre & post (during the shift if people share equipment) work shift (preventing transmission through sharing of equipment during shift change; that's equipment such as drilling machines, mobile equipment (steering wheels, gear knobs), computers in control rooms,control panels, etc. that are shared through different shifts), especially surfaces that will be frequently touched (The Original Equipment Manufacture instruction must be consulted prior to disinfecting such equipment to prevent any damage or deterioration of such equipment). |
| (d) | Cough in the fold of the elbow or in a tissue which you discard and wash your hands. |
| (e) | Avoid touching your eyes, nose and mouth with unwashed hands. |
| (f) | Wearing of fabric face mask in public places rather than using medical masks reserved for healthcare workers can assist in slowing the spread of the coronavirus, but that other hygiene measures are also crucial. |

| 5. | RESPIRATORY PROTECTIVE EQUIPMENT (RPE) APPLICATION AGAINST COVID-19 |
A continuing, effective respiratory protection program as specified by applicable local regulations must be implemented when using Respiratory Protective Equipment (RPE) as a control.
| (a) | De-densified and social distanced areas |
In areas where de-densification and social distancing (with clearly demarcated standing, seating or working position/s) has been achieved, the use of face masks (surgical masks) is optional while cloth masks are recommended, in accordance with guidance from relevant legislative requirements and/or the appointed Section 12 Occupational Hygiene and Ventilation Engineer.
| (b) | Non de-densified and social distanced areas |
In workplace areas or situations where de-densification and social distancing can't be achieved to protect workers from exposure to respiratory droplets that may be carrying COVID-19 viruses, and where the use of industrial RPE (typically FFP2 respirators or cartridge type respirators for gas/fume and particulate mitigation) is compulsory for protection against airborne particulates, the RPE can double-up as protection against COVID-19 by reducing the spread of respiratory droplets.No need for additional masks.
Where industrial respiratory protection is not used or available and mine workers are crowded in confined areas the use of face masks (surgical masks) is recommended, in accordance with guidance from relevant local authorities and/or the appointed Section 12 Occupational Hygiene and Ventilation Engineer.
| (c) | "COVID-19 Mask Zones" |
Mines should identify the potential high-risk areas and tasks which social distancing is not possible, for example shaft conveyances (mine cages), underground man carriers, etc. and demarcate these as "COVID-19 mask zones". Employees should not be allowed in such demarcated areas without a respirator or facial mask.
Note: The use of cloth masks is under investigation, but for the interim, considering the potential risk posed by not being able to practice social distancing, surgical masks are recommended for use In crowded workplaces.
| (d) | Safe Disposal of RPE |
| √ | Put the used RPE in a dedicated rubbish waste bag/s and seal the rubbish waste bag when it's full; |
| √ | Store the full sealed rubbish waste bag in a dedicated storage area; |
| √ | The sealed rubbish waste bag with face masks should be stored for a period not less than 48 hours prior to being disposed of in the local waste; |
| √ | The sealed rubbish waste bag with industrial RPE should be stored for a period not less than 7 days prior to being disposed of in the local waste; and |
| √ | local waste disposal requirements must be followed. |
Note: The mine should keep a record of the type of RPE being disposed, when the full rubbish waste bag was sealed and when was such full rubbish waste disposed of in the local waste.
| 6. | GENERAL GUIDANCE INFORMATION ON PPE |
Respiratory protection
The respirator protects individuals from the inhalation of droplets and particles but also reduces the spread of infectious respiratory droplets. Given that the fitting of different types of respirator will vary for each user, the respirator will require a fit testing in order to find the best fit PPE to the user. In the event of the need to assess a suspected case of COVID-19 or in the management of such a confirmed case of COVID-19, the guide suggests the use of Filtering Face Piece (FFP) respirators class 2 or 3 (FFP2 or FFP3) (N95). An FFP3 respirator should always be used when performing aerosol-generating activities/procedures.
When not in use, i.e. in the workplace where inhalable hazards are absent and where social distancing can be practised, mine workers should be provided with the means to store the RPE (for example, a sealable plastic bag) to prevent contamination when the mask is not in use.
Eye protection
Eye and face protection provide protection against contamination to the eyes from respiratory droplets arising from aerosol generating procedures and from splashing of secretions (including respiratory secretions), blood, body fluids or excretions in the health care environment. Pertaining to COVID-19 eye protection is only required by Healthcare workers, EMS personnel, COVID-19 Site Screening Teams and Cleaners who might came into contact with respiratory droplets. (high risk group)
Eye and face protection can be achieved using any one of the following:
| • | surgical mask with integrated visor |
| • | full face shield or visor |
| • | polycarbonate safety spectacles or equivalent |
Body protection
In instances where very high-risk procedures are conducted, body protection in the form of gowns and plastic aprons will be required.
Gloves
Surgical (disposable but not theatre grade) gloves must be worn when providing direct patient care and when exposure to blood and or other body fluids is anticipated or likely, including during equipment and environmental decontamination. Disposable gloves are subject to single use and must be disposed of immediately after completion of a procedure or task and after each patient contact, followed by the application of hand hygiene.
Gloves provided as part of PPE for a specific occupation will continue to be utilised. Good storage of gloves should be promoted. In case of reusable gloves, they should be washed and decontaminated at end of the shift and hang to dry for next shift use.
Note: Gloves are not required as general protection against the COVID-19 virus for occupations and tasks not described above.
| 7. | CLOTH FACE MASKS (UNDER INVESTIGATION) |
There is good evidence to show that cloth face masks significantly reduce the spread of infectious respiratory droplets. Through lowered amounts of exhaled Coronavirus, wearing a mask should reduce the spread of infection from the wearer's respiratory droplets. Although a cloth face mask may not be as good as a surgical face mask in hospital settings, the cloth face mask is a suitable alternative to surgical face masks to reduce droplet spread. Hence, cloth face masks are recommended for situations where social distancing is not possible and respiratory protection for protection against inhalable hazards is not required.
Face masks are recommended in addition to hand-washing and social distancing - it does not replace these two more important strategies. Cloth face mask should never be promoted as a primary prevention strategy and be used in accordance with guidance from relevant local authorities.
N95 respirators and surgical medical masks are reserved for health workers and suspected infected COVID-19 cases.
FFP2 (or similar) respirators are reserved for workers in respirator zones to prevent exposure to inhalable particulate hazards in the workplace
Cloth face masks can be used when an individual comes into contact with people and social distancing can't be maintained like when using public/bus transport, attending essential services, general public use, etc. Cloth face masks should always be accompanied by clear user instructions on strict mask use (donning, doffing, disposal,etc.) and hygiene. Could also be used for suspected infected COVID-19 cases.
Cloth face masks should—
| • | fit snugly but comfortably against the side of the face; |
| • | cover the nose and mouth completely; |
| • | be secured with ties or ear loops; |
| • | include multiple layers of fabric; |
| • | allow for breathing without restriction; and |
| • | be able to be laundered and machine dried without damage or change to the shape |
Face masks should not be lowered when speaking, coughing or sneezing. Face masks should not be repeatedly touched - fiddling with the mask repeatedly is strongly discouraged as it is important to avoid touching the face with hands.The inner side of the mask should not be touched by hands.
It is important to wash hand first before putting on the face mask. Individuals should be careful not to touch their eyes, nose, and mouth when removing their cloth face mask and wash their hands after removing the cloth face mask. Wash cloth face masks with warm water (60-90°C (140-194°F)] common household detergent, and dry thoroughly. If possible, iron the mask after washing as it will help with disinfection. Each person will need to have at least two face masks so that one face mask is available when the other is being washed.
Cloth face masks must be accompanied with instructions to the Wearer of the mask. As minimum, the instructions must cover the following points:
| • | The importance that masks are used in addition to control measures such as hand washing, social distancing, etc. |
| • | Washing the hands with soap and water or an alcohol-based hand rub before handling and putting on the mask |
| • | To cover the nose and the mouth with the mask and to make sure that there are no obvious gaps between the mask and the wearers face. |
| • | Avoid touching the mask when using it. If the mask needs to be touched or adjusted, wash hands with soap and water or an alcohol-based hand rub after touching the mask. This also applies when the mask is removed. |
A cloth mask of acceptable standard and design must consist of three layers:
| • | Outer layer (faces towards other people): made from thick weave cotton like denim, calico, upholstery fabric, etc. Must be water repellent, easy to clean and be quick drying |
| • | Inner layer (against the face): Can be made with the same material as the outer layer. Both polyester and nylon fabrics are preferred. Cotton can be used but this fabric can be highly water absorbent and become wet against skin. |
| • | Middle/Filter layer: using the same fabric as inner/outer layer or fabric that is used in lining of suit jackets or formal coats. The layer could also be gauze from the pharmacy (non-woven), dried out wet wipes (unscented), or brand-new polyester floor wipes (dry ones). It is recommended that the non-woven layer be replaced daily with a fresh one and not be reuse. |
| o | Avoid T-shirt material. |
| o | Use fabrics that can be washed in hot water and ironed. |
| • | Cleaning and disinfection instructions |
Cloth masks for health care workers. Cloth masks are not recommended for health care workers because there is no filtration or protection against droplets or splashes. There is also the "wicking effect" which increases the risk of mucous membrane contamination.
Cloth masks for source isolation (community). As there is an urgent need to preserve essential PPE, especially face masks for healthcare workers, the use of cloth masks may be considered for source Isolation for community healthcare workers, security, and the general public particularly when travelling in enclosed spaces such as taxis.
| 8. | REPLACEMENT AND EXTENDING THE USE OF RPE |
Respirators are for single use or single session use and then are to be discarded (hand hygiene must always be performed after disposal) or if re-usable cleaned accorded manufacturer's instructions. It is important that the respirator maintains its fit,function and remains tolerable for the user.
The respirator should be discarded and replaced and NOT be subject to continued use in any of the following circumstances:
| • | is damaged |
| • | is soiled (for example, with secretions, body fluids) |
| • | is damp |
| • | facial seal is compromised |
| • | is uncomfortable |
| • | is difficult to breathe through |
The manufacturers' guidance should be followed in regard to the maximum duration of use.
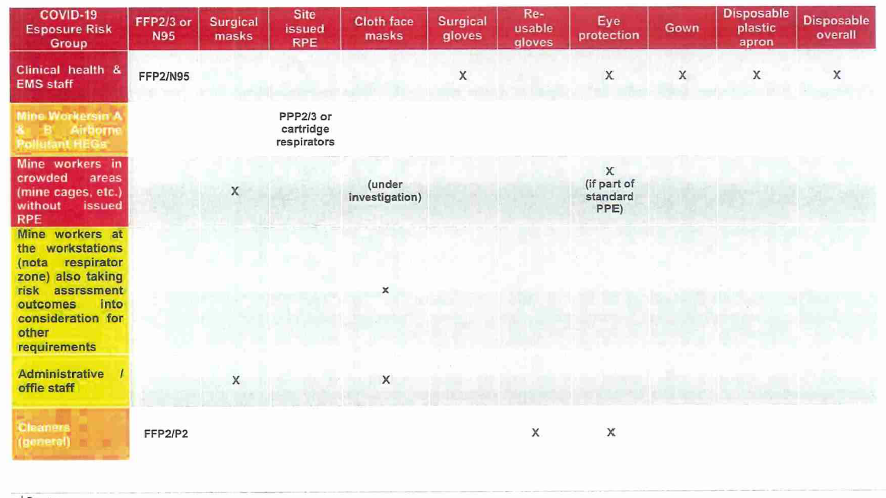
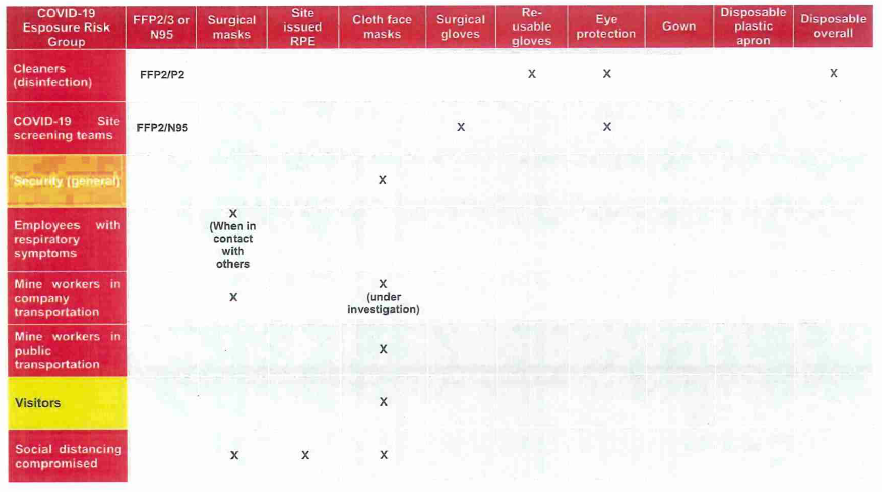
A summary of the recommended PPE for each category of worker is provided in section 10
| 9. | COVID-19 POTENTIAL EXPOSURE GROUPS AND PPE |
| 10. | REFERENCES |
National Department of Health. COVID-19 Infection Prevention and Control Guidelines for South Africa, March 2020
National Department of Health. National Practical Manual for the Implementation of the National IPC Strategic Framework, March 2020
Circular H25/20: Guidelines for PPE during coronavirus disease 2019 (covid-19) Western Cape Government: Health March 2020
South Africa Occupational Health and Safety Act, Act 85 of 1993 - Regulations for Hazardous Biological Agents, 2001.
WHO Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19), March 2020.
ECDC Technical Report- Personal protective equipment (PPE) needs in healthcare settings for the care of patients with suspected or confirmed novel coronavirus (2019-nCoV), February 2020.
UK Public Health: COVID-19 personal protective equipment (PPE), April 2020
https://www.who.int/emergencies/diseases/novel-coronavirus-2019
https://www.cdc.gov/coronavirus/2019-ncov/prevent-gettinq-sick/diy-clothface-coverings.htmI
https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causinq-covid-19-implications-for-ipc-precaution-recommendations
https://www.who.int/publications/i/item/covid-19-and-food-safety-guidance-for-food-businesses