


National Health Act, 2003 (Act No. 61 of 2003)NoticesNational Health Insurance Policy towards Universal Health CoverageChapter 7 : Financing of NHI7.3 NHI Expenditure Projections: and Cost Estimates7.3.1 NHI Expenditure Scenarios |
| 202. | The projections set out in the Green Paper were derived from a model of aggregate costs built on projected utilisation based on demographic trends. A revised version of these projections is summarised in Table 1, based on more recent estimates of the costs of the NHI pilots and other reforms currently being implemented. In this scenario, total NHI costs in 2025 are shown as R256 billion (in 2010 terms) as in the Green Paper, but the cost increase in the early years is more moderate. |
Table 1: Projection of NHI costs adapted from Green Paper
|
Average annual per cent real increase |
Cost Projection R m(2010 prices) |
|
Baseline public health budget: |
2010/11 |
|
109 769 |
Projected NHI expenditure: |
2015/16 |
4.1% |
134 324 |
2020/21 |
6.7% |
185 370 |
|
2025/26 |
6.7% |
255 815 |
|
Funding shortfall in 2025/26 if baseline increases by: |
2.0% 3.5% 5.0% |
108 080 71 914 27 613 |
|
Source: National Treasury projection (2012)
| 203. | In this projection, NHI expenditure increases by 6.7 per cent a year in real terms after 2015/16, resulting in a cost projection in 2025/26 of R256 billion in 2010 prices. These projections would take the level of public health spending from around 4 per cent of GDP currently to 6.2 per cent of GDP by 2025/26, assuming the economy grows at an annual rate of 3.5 per cent. This increase would be below the level of public spending (as a percentage of GDP) of many developed countries. |
| 204. | There are many factors that influence health expenditure. These include trends in population health service needs and utilisation (e.g. epidemiological trends, rates of hospitalisation and use of outpatient services). It also depends on supply capacity, such as availability of health facilities and professional personnel as well as the prices of supplies and services. Policy options that will impact on costs include the range of private service providers from whom services are purchased and the reimbursement arrangements. Costs will also depend on the extent to which economies of scale are achieved through active purchasing and the effectiveness of cost controls. |
| 205. | In making long-term forward estimates of health service expenditure, it must be anticipated that medical costs will rise over time - independent of NHI implementation - because of factors such as population ageing, technological advances and higher demand for healthcare. Total health expenditure growth will be influenced by expansion of comprehensive healthcare services, the extent to which users come to trust the health services covered by the NHI Fund and choose to reduce voluntary health insurance cover. |
| 206. | The main cost estimate used by the National Treasury for the purposes of modelling revenue raising options is presented here. These are set out in 2010/11 constant prices and can be compared with the public health spending baseline of around R110 billion in 2010/11. It must be stressed that these are illustrative projections and do not represent the actual expenditure commitments that will occur from the phased implementation of NHI. Figure 2 illustrates the funding shortfall for alternative baseline resource growth projections. |
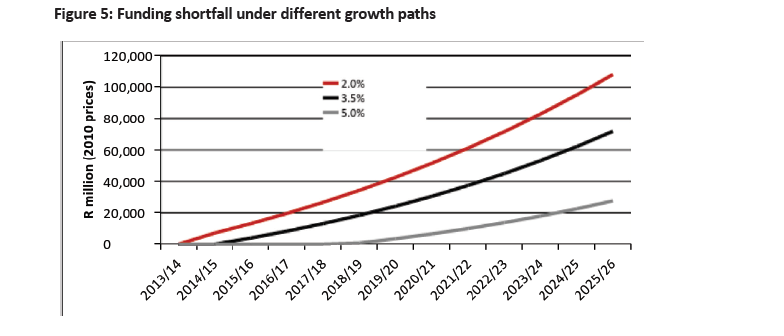
| 207. | The funding shortfall is R71.9 billion in 2025/26 if the baseline increases by 3.5 per cent a year. It would be R27.6 billion if baseline resources grow by 5.0 per cent a year (in real terms) and would be R108 billion if baseline resources grow by 2.0 per cent per year. Over the long run, the pace of economic growth is an important indicator of overall growth rate in health expenditure. |
| 208. | This projection also does not take into account the health system’s absorptive capacity and personnel requirements or the dynamics of the accompanying public and private sector health service reforms. As people make greater use of health services under NHI, their expenditure on private health services would decrease. |